Genetic changes that cause cancer can be inherited or arise from specific environmental exposures. Genetic changes can also happen because of errors that occur as cells divide.
Credit: National Cancer Institute, USA
Is cancer a genetic disease?
Yes, cancer is a genetic disease. It is caused by gene changes that control how cells grow and multiply. Cells are the building blocks of the body. Each cell has a copy of the genes. Genes are sections of DNA that carry instructions to make a protein or several proteins. Scientists have found hundreds of DNA and genetic changes (variants, mutations, or alterations) that help cancerous cells form, grow, and spread.
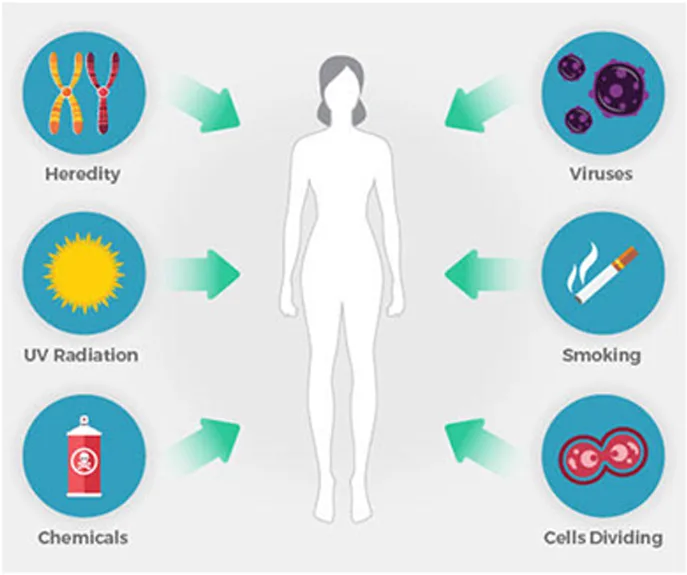
Cancer-related genetic changes can occur because:
- Random errors occur as the cells multiply in our DNA
- The DNA is altered by carcinogens in our environment, such as chemicals in tobacco smoke, UV rays from the sun, and the human papillomavirus (HPV)
- They were inherited from one of our parents
DNA changes can happen throughout our lives and even in the womb, whether caused by a random mistake or a carcinogen. While most genetic changes aren't harmful, accumulating genetic changes over many years can turn healthy cells into cancerous cells. Most cancers occur by chance due to this process over time.
Credit: National Cancer Institute, USA
Multiple kinds of genetic changes can lead to cancer. One genetic change, called a DNA mutation or genetic variant, is a change in the DNA code, like a typo in the sequence of DNA letters. Some variants affect just one DNA letter, called a nucleotide. A nucleotide may be missing, or another nucleotide may replace it. These are called point mutations.
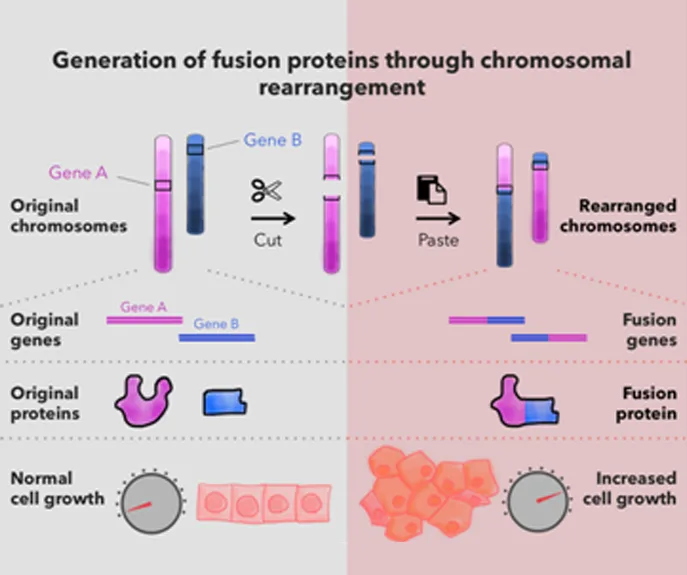
Cancer-causing genetic changes can also occur when segments of DNA — sometimes very large ones — are rearranged, deleted, or copied. These are called chromosomal rearrangements.
Some cancer-causing DNA changes occur outside genes, in sections of DNA that act like “on” or “off” switches for nearby genes. For example, some brain cancer cells have multiple copies of “on” switches next to genes that drive cell growth.
Other DNA changes, known as epigenetic changes, can also cause cancer. Unlike genetic variants, epigenetic changes (sometimes called epimutations) may be reversible and they don’t affect the DNA code. Instead, epigenetic changes affect how DNA is packed into the nucleus. By changing how DNA is packaged, epigenetic changes can alter how much protein a gene makes.
Some substances and chemicals in the environment that cause genetic changes can also cause epigenetic changes, such as tobacco smoke, heavy metals like cadmium, and viruses like Epstein-Barr virus.
Credit: National Cancer Institute, USA
Is cancer hereditary?
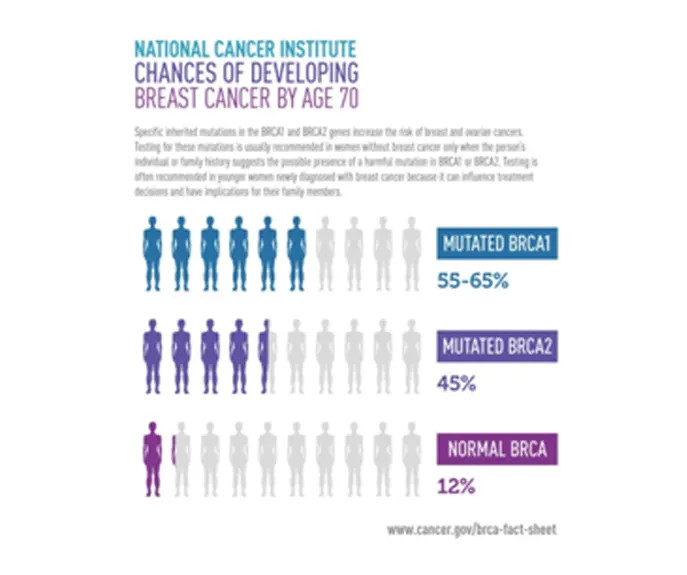
Cancer itself can't be passed down from parents to children. And genetic changes in tumour cells can't be passed down. But a genetic change that increases the risk of cancer can be passed down inherited if present in a parent's egg or sperm cells.
For example, suppose a parent passes a mutated BRCA1 or BRCA2 gene to their child. In that case, the child will have a much higher risk of developing breast and several other cancers.
That's why cancer sometimes appears to run in families. Inherited genetic changes may cause up to 10% of all cancers. Inheriting a cancer-related genetic modification doesn't mean you will get cancer. It means that the risk of getting cancer is increased for you.
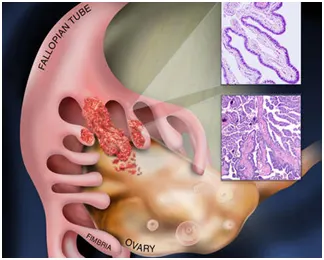
Cancers in Women
Breast cancer |
Ovarian cancer |
Cervical cancer |
Endometrial cancer |
Lung cancer |
Skin cancer |
Colorectal cancer |
How does Genome Foundation help in identifying cancer risks?
Certain genetic tests can show if you’ve inherited a genetic change that increases your risk of cancer. This testing is usually done with a small sample of blood, but it can sometimes be done with saliva, cells from inside the cheek, or skin cells.
Genetic tests can help families with a history of breast and ovarian cancer make screening and treatment decisions. Not everyone needs to get genetic testing for cancer risk. Your doctor or health care provider can help you decide if you should get tested for genetic changes that increase cancer risk. They will likely ask if you have certain patterns in your personal or family medical history, such as cancer at an unusually young age or several relatives with the same kind of cancer.
If your doctor recommends genetic testing, talking with a genetic counsellor can help you consider the potential risks, benefits, and drawbacks of genetic testing in your situation. After testing, a genetic counsellor, doctor, or other health care professional trained in genetics can help you understand what the test results mean for you and your family.
Although it's possible to independently order an at-home genetic test, these tests have many drawbacks. They are not generally recommended as a way to see whether you have inherited a genetic change that increases cancer risk.
In other words, Genome Foundation offers “Personalized medicine." This means you will be offered medical care based on your own personal or individual body cells and genes that can cause specific disease and Genome Foundation provides thorough personalised in-depth study of such genes that may cause or likely to cause cancer.
Personalized cancer medicine comes from studies of human genes and the genes in different cancers. These studies have helped researchers design more effective treatments. They have also used genetic information to develop tests for cancer and ways to prevent it. This is because it is designed to be more specific. A tailored treatment may have fewer side effects on healthy cells and more on cancerous cells.
At Genome Foundation, for a personalised cancer screening or cancer treatment plan, we include the following:
- Learning your chances of developing cancer and choosing screening tests to lower the risk.
- Matching the treatment to your genes and your cancer's genes. This may be more effective and cause fewer side effects.
- Predicting how likely the cancer is to come back. Doctors call this "risk of recurrence."
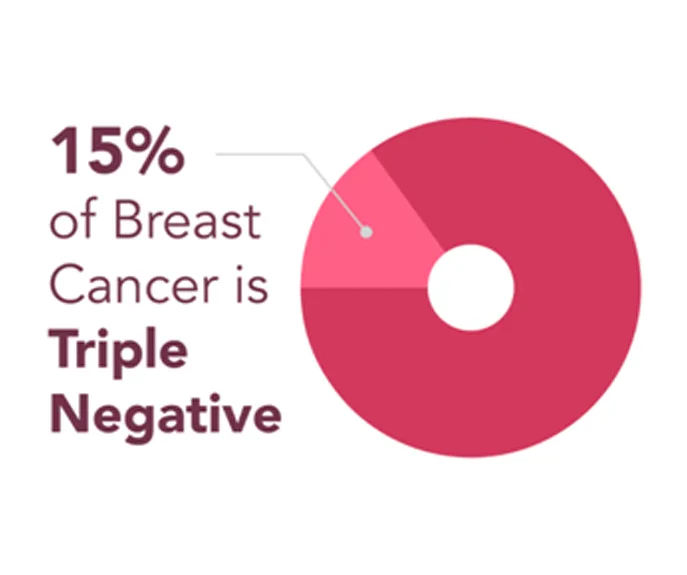
Credit:National Breast Cancer Foundation, Inc., USA.
Core research project in progress at Genome Foundation
Genome Foundation in collaboration with KIMS Hospitals, Basavatarakam Indo-American Cancer Hospital & Research Institute, Hyderabad and Mahatma Gandhi Cancer Hospital & Research Institute, Vishakhapatnam is working on “Genomic Profiling of Indian women with Triple Negative Breast Cancer (TNBC).” TNBC refers to the fact that the cancer cells do not have estrogen or progesterone receptors (ER or PR) and also do not make any or too much of the protein called HER2. The aim of this study is to:
- Compare metastatic vs non-metastatic and BRCA positive vs BRCA negative TNBC;
- Clinical correlation of results to identify clinically potent variants (diagnostic/prognostic/preventive markers) and
- Identify germ-line and tumour specific somatic variants (Analysing the variants in genomic DNA isolated from corresponding blood samples and correlating with expressed genes (qPCR analysis using RNA isolated from tissues stored in Trizol).